When it comes to women’s health, there’s a lot of jargon to wade through. One term you might have come across is ‘myomectomy’. But what exactly is it? Why is it performed? If these questions are swirling in your mind, you’re in the right place.
This article aims to demystify myomectomy, a surgical procedure often overshadowed by its more well-known cousin, the hysterectomy. We’ll delve into its ins and outs, helping you understand when it’s used, and what you can expect if you’re facing one.
So, whether you’re a patient, a loved one, or just someone who’s curious about women’s health, stick around. You’re about to get a clear, concise, and comprehensive look at myomectomy.
Myomectomy, a surgical operation, works to remove uterine fibroids—non-cancerous growths appearing in the uterus during childbearing years of a woman’s life. Unlike a hysterectomy, this procedure aims to eradicate the fibroids while preserving the uterus, maintaining a woman’s fertility.
Myomectomy Types
Three distinct types of myomectomy procedures exist: Abdominal Myomectomy, Laparoscopic Myomectomy, and Hysteroscopic Myomectomy.
- Abdominal Myomectomy: Surgeons employ this technique when fibroids are large or numerous. It involves a single, large incision in the belly area.
- Laparoscopic Myomectomy: It’s best for smaller fibroids that are located towards the outside of the uterus. Surgeons make several small incisions in the lower abdomen.
- Hysteroscopic Myomectomy: It’s optimal for removal of submucosal fibroids—the ones that project into the uterus. The physician uses a hysteroscope inserted through the vagina and cervix.
Surgeons in Melbourne, for example, select the type of myomectomy based on the size, number, and location of the fibroids.
Procedure Steps
The exact process may vary slightly depending on the kind of myomectomy. However, in essence, a surgeon makes an incision, locates and removes the fibroids, then sews the uterus back together.
Prior to removal, areas around the fibroids are injected with a medication to reduce blood loss. Post operation, the patient’s recovery period can differ depending on the procedure type, with laparoscopic and hysteroscopic myomectomy usually offering quicker recovery times.
Risks and Postoperative Care
While myomectomy is typically a safe procedure, any surgery carries potential risks. Complications can include infection, blood clot formation, or damage to the uterus. Specific to myomectomy, there’s a potential for recurrence of fibroids.
Postoperative care also varies by the type of procedure. A hospital stay may be necessary after an abdominal myomectomy. Conversely, laparoscopic or hysteroscopic myomectomies often allow the patient to return home the same day. The managing of pain and the decision to be pregnant again are typically discussed with the patient’s healthcare provider post-operation.
What Is Myomectomy?
Myomectomy stands as a selectively targeted surgical operation that primarily aims at removing uterine fibroids without disturbing or damaging the uterus. This surgery, thus, maintains the reproductive health and fertility of a woman.
Types of Myomectomy Procedures
Three types of myomectomy procedures are in common clinical practice. The Abdominal Myomectomy involves a substantial incision in the abdominal area for fibroid removal. It’s particularly useful for treating large-scale, numerosity of fibroids. Doctors execute the Laparoscopic Myomectomy by introducing small incisions and inserting a laparoscope for fibroid eradication. It usually suits smaller fibroids that reside on the outer surface of the uterus. The Hysteroscopic Myomectomy uses a hysteroscope that is inserted through the vagina to address fibroids in the uterus’ inner lining. This procedure mainly suits submucosal fibroids. Notably in Melbourne, these three myomectomy procedures are offered to patients depending on their specific case.
When Is Myomectomy Recommended?
Specialists typically propose a myomectomy when other non-surgical treatments fail to provide relief from symptoms related to fibroids. If the patient experiences heavy menstrual bleeding, pelvic pain, and pressure, or if fibroids impede fertility, a myomectomy becomes an operative recommendation. Also, a woman desiring to get pregnant in the future but having uterine fibroids would probably get a recommendation for a myomectomy. These criteria serve as the primary considerations observed by physicians in Melbourne when deciding on the myomectomy procedure.
Preparing for Myomectomy
Acquiring knowledge about preoperative preparations for a myomectomy can combat uncertainty and potentially assuage any fears a patient might have. In-depth prep includes both the initial consultations and tests, followed by specific pre-surgery instructions.
Initial Consultation and Tests
A patient’s journey usually begins with an initial consultation, where the surgeon providing the myomectomy procedure in Melbourne thoroughly assesses their health history, present overall condition and the nature of the fibroids. Further, diagnostic tests like ultrasound, MRI and sometimes hysteroscopy are conducted to ascertain the size, location, and number of fibroids. Blood tests ensure the patient’s readiness for surgery and an anesthesiologist evaluates fitness for anesthesia.
Pre-Surgery Instructions
Following the initial consultation and tests, patients receive detailed pre-surgery instructions. These include a directive to fast for eight hours prior to surgery and an advice to shower using antibacterial soap on the morning of the surgery. Usage of certain medications need to be stopped a week before the operation, if the surgeons deem it necessary, with an optimal replacement medication regime suggested.
It’s also recommended that arrangements are made for postoperative support, as mild discomfort or fatigue is expected post-surgery. These instructions are a quintessential part of preparing for a myomectomy and patients are encouraged to adhere strictly to them.
The Myomectomy Procedure
Diving into specifics, let’s explore the journey of undergoing a myomectomy procedure in Melbourne. Following the selection of the appropriate method, the surgical procedure is carried out with precision and care, keeping patient safety and comfort as the priority.
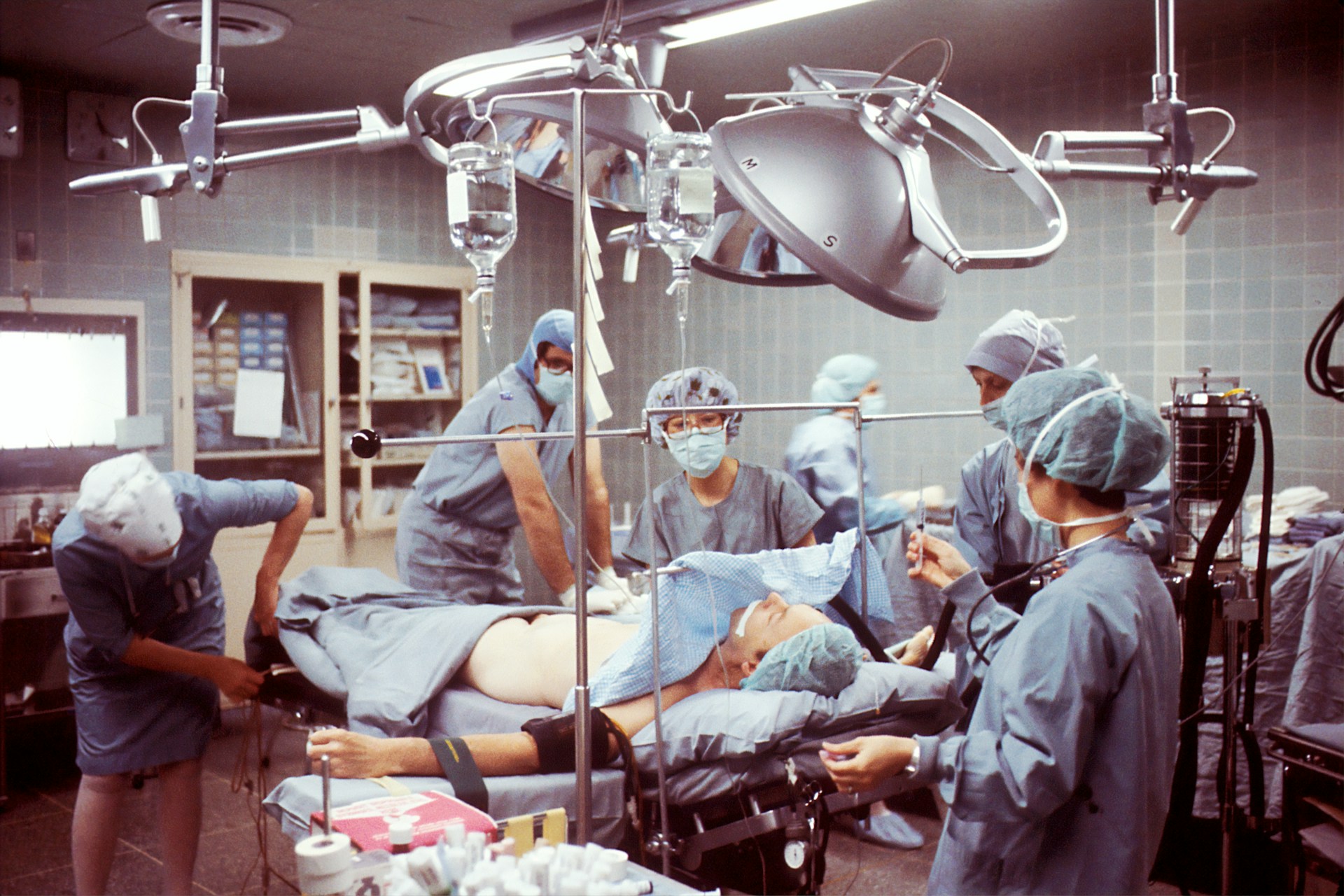
During the Surgery
Once the patient is under anesthesia, the surgical team gets to work with the procedure. In the case of an abdominal myomectomy, surgeons make a sizeable incision into the lower abdomen, providing direct access to the fibroids. Conversely, laparoscopic and hysteroscopic myomectomies involve smaller incisions and specialized instruments to reach and remove these growths. Throughout the surgery, surgeons constantly monitor the patient’s vital stats, and manage bleeding efficiently.
Post-removal of fibroids, meticulous suturing ensures the integrity of the uterus, optimizing its potential for future pregnancies. The length of the surgery varies, typically lasting between one to three hours depending on fibroid characteristics and individuals’ health conditions.
Technologies and Techniques Used
Embracing advancements, the myomectomy procedure in Melbourne employs state-of-the-art technology and techniques. Laparoscopic procedures, for instance, utilize high-resolution cameras and delicate instruments managed through small incisions. These tools offer enlarged, clear visuals of the uterus and fibroids, facilitating precision in the procedure.
On the other hand, hysteroscopic myomectomies utilize a slender device called a hysteroscope, inserted through the vagina and cervix into the uterus. This technique allows for a no-incision approach to fibroid management.
In cases where fibroids are deeply embedded, surgeons may use advanced imaging techniques, such as intraoperative ultrasound, to assist in the identification and extraction of fibroids. These technological enhancements not only improve surgical outcomes but also contribute to shorter hospital stays and quicker recovery periods for patients.
Recovery After Myomectomy
Recoveries after a myomectomy procedure entail both immediate post-surgery care and long-term healing strategies. Both these phases demand equal attention to ensure a successful healing process.
Immediate Post-Surgery Care
Immediately following a myomectomy conducted in Melbourne, pain control forms the priority. Doctors use a combination of medications, both oral and intravenous, to manage post-surgical discomfort. Typically, patients remain under observation in the hospital for at least 24 hours to monitor for any potential complications like bleeding or infection. If a laparoscopic or hysteroscopic method is employed, the discharge might occur sooner. Apart from pain management, practitioners also focus on preventing thrombosis, a condition where blood clots form in the deep veins. Implementing early mobilization and use of low-molecular-weight heparin help in decreasing the risk.
Long-Term Healing and Care
Long-term care after a Melbourne myomectomy is primarily guided by the procedure’s type, patient’s health status, and the surgeon’s recommendations. Follow-up appointments are critical and usually scheduled during the first and sixth week post-surgery. Wound care and gradual reintroduction of normal activities are essential parts of the recovery process. For instance, lifting heavy objects and engaging in strenuous exercises are typically avoided for six weeks post-surgery. Likewise, sexual activities and tampon usage are avoided until the doctor gives clearance, usually around four to six weeks following the procedure.
Post-surgery, keeping up with moderate exercises, such as walking, enhances circulation and aids wound healing. Physical rehabilitation may be recommended in some cases.
A healthy and balanced diet assists in managing weight, preventing constipation, and fostering healing. Patients are advised to not let their nutrition slide, emphasizing high fiber foods, staying hydrated, and avoiding alcohol and caffeine.
Patients need to stay vigilant for post-surgical complications signs, like severe pain, fever, heavy bleeding, or wound complications. The presentation of any of these symptoms warrants immediate medical attention. Regular follow-ups with the surgeon or gynecologist help the patient stay abreast of their healing progress, making necessary adjustments to the recovery plan when needed.

Each recovery journey from a myomectomy is unique, and it’s crucial to remember that recovery rates will differ for everyone. Patience and adherence to the prescribed medical plan will, however, ensure an optimal healing process.
Risks and Complications of Myomectomy
Comprehensive knowledge about the risks and complications related to the myomectomy procedure is equally crucial for proper patient preparation. Let’s first take a look at the immediate complications that can occur.
Common Immediate Complications
While medical professionals in Melbourne employ various advanced tools and techniques to ensure a smooth myomectomy procedure, immediate post-operative complications are possible. Defining these risks are blood loss and infection. Excessive bleeding during surgery remains a concern due to the extensive vascular system that feeds the fibroids. Should excessive blood loss become uncontrollable, conversion to a hysterectomy might be required, though rare. An infection, a relatively uncommon occurrence following a myomectomy, could develop in the wound, urinary tract, or within the body where the fibroids were once located.
Potential Long-Term Effects
Emphasis should be placed on the broader temporal scope, too – potential long-term effects of a myomectomy. One such long-term effect includes potential difficulties with childbirth. In some cases, the incisions made during an abdominal myomectomy can complicate pregnancy, potentially leading to a necessity for a cesarean delivery. Adhesion development, where internal scar tissue forms and binds nearby organs together, is another potential long-term effect. While not necessarily life-threatening, adhesions can lead to chronic pelvic pain and potential fertility issues. Lastly, regrowth of fibroids might occur, particularly in younger women with numerous fibroids initially mandating continued long-term monitoring.
So, whether you’re a patient in Melbourne or elsewhere, understanding myomectomy in depth helps you make informed decisions about your health.
