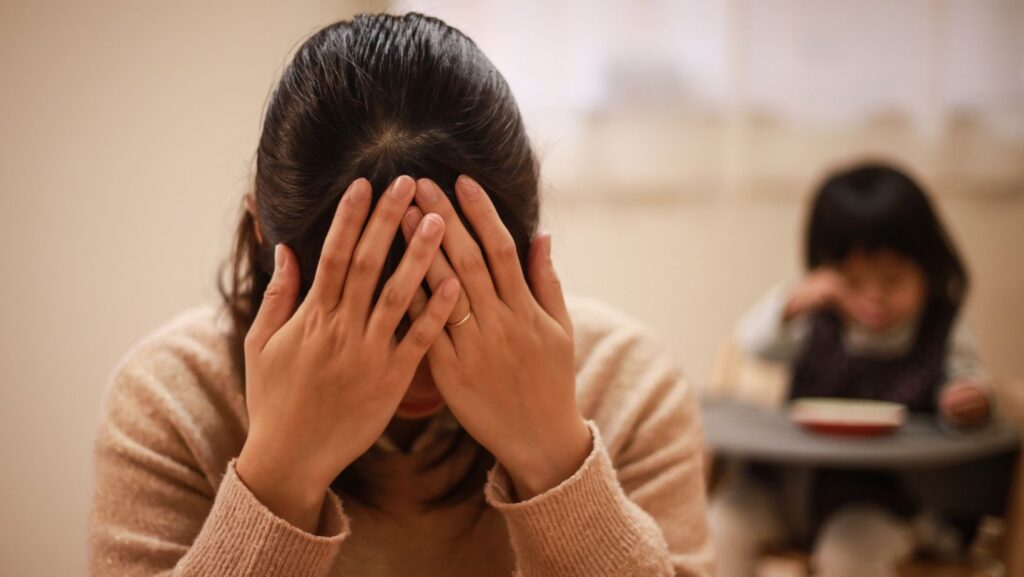
The quiet weight many mothers carry
Most stay-at-home mothers know the exhaustion that comes from juggling endless tasks—laundry, meals, emotional support, and invisible work that keeps the family running. But beneath that daily fatigue, some moms experience something deeper: aching muscles, tension headaches, and a fog that won’t lift. What’s often dismissed as “just stress” could actually be part of a bigger picture—one that connects hormonal shifts, chronic pain, and undiagnosed ADHD.
How the body and mind react to constant strain
Chronic pain and stress form a two-way loop. Stress releases cortisol and adrenaline, which tighten muscles and heighten sensitivity to pain. Over time, the body forgets how to relax, and pain becomes the new normal. Researchers studying the overlap between ADHD and chronic pain have found that attention dysregulation and pain processing share common brain pathways. When mental overload meets physical strain, the nervous system stays on high alert—exactly what many mothers experience daily.
Add emotional labor—the mental load of remembering everything from doctor appointments to what’s running low in the pantry—and you have a perfect storm for pain and burnout.
Why stay-at-home moms feel it more
Home life might seem less demanding than a full-time job, but anyone who’s done it knows it’s a 24/7 role. The combination of physical chores, emotional caretaking, and limited recovery time keeps stress hormones active.
Fluctuating estrogen levels throughout the menstrual cycle and after childbirth also affect pain sensitivity and attention regulation. When estrogen dips, pain tolerance can drop too, leading to sharper aches and emotional volatility.
These shifts often mask or mimic ADHD symptoms. That’s one reason why ADHD is more challenging for women—their distractibility and irritability are often blamed on hormones or motherhood, not a neurological condition.
How stress and hormones make pain worse
Cortisol—the body’s main stress hormone—can heighten inflammation and disrupt sleep, two triggers that intensify pain. When cortisol stays elevated, muscles don’t fully relax, leading to tension headaches, neck tightness, or stiffness through the shoulders and back.
Estrogen interacts with serotonin and dopamine, the same neurotransmitters linked to ADHD. When estrogen dips, it can worsen focus and emotional balance. For mothers already dealing with overwhelm, this creates a cycle where hormonal changes amplify both pain and cognitive fatigue.
Doctors sometimes recommend topical or localized anti-inflammatory options for safety, especially while breastfeeding. Current NHS guidelines note that some NSAIDs can be used cautiously during breastfeeding, with proper supervision and medical advice.
Common pain patterns among mothers
Many moms describe the same recurring issues: headaches that start behind the eyes, tension through the neck, or a burning ache in the middle of the back after a long day of bending and lifting. That middle of back pain can stem from muscle strain, poor posture, or carrying toddlers on one hip all day.
For some, pain comes with sudden migraines that shut down the whole evening routine. Gentle, non-invasive solutions—like using a cooling roll-on or menthol-based topical—can provide short-term relief. One example is MEDISTIK instant migraine relief, a topical approach designed for quick comfort without relying solely on oral painkillers. Combined with stretching, hydration, and downtime, these small steps help reduce intensity and frequency of attacks.
When “stress” is actually undiagnosed ADHD

For years, women have been underdiagnosed with ADHD because their symptoms don’t always look like the hyperactive stereotype. Instead, they appear as chronic disorganization, emotional outbursts, forgetfulness, or mental fatigue—traits often mislabeled as “just stress.”
Undiagnosed ADHD can make pain management even harder. Impulsivity can lead to inconsistent self-care, and racing thoughts prevent real rest. Accessible screening tools, such as ADHD online, can guide mothers toward understanding whether attention issues play a role in their exhaustion.
For a simple first step, a free ADHD test can help identify common symptoms worth discussing with a healthcare provider. Early awareness helps mothers make sense of what’s happening in both mind and body, instead of internalizing guilt for not “keeping up.”
Practical, holistic ways to manage daily pain
Managing chronic pain doesn’t always mean starting medication right away. Small, consistent actions can make a big difference.
- Structure and rest
Creating predictable routines helps calm the nervous system and supports ADHD management. Short breaks, gentle stretching, and realistic expectations reduce muscle tension and cognitive overload. - Nourishment and energy
A balanced diet helps regulate hormones and energy. Moms who often skip meals can fill nutritional gaps with something convenient like a great greens powder—a way to get essential nutrients without another task on the list. - Emotional grounding through animals
Many families notice calmer moods and reduced anxiety after spending time with pets. Scientific reviews show companion animals can lower blood pressure and increase serotonin. For mothers navigating ADHD and chronic pain, an emotional support animal can be a comforting part of mental health care. - Smart body mechanics
Think of body alignment like a putting grip—small adjustments change everything. Standing tall, bending from the knees, and shifting weight evenly prevent repetitive strain in the back and shoulders. - Local pain relief and mindfulness
Topical options like roll-ons or sprays help target sore spots without systemic side effects. According to MEDISTIK’s clinical insights, menthol and methyl salicylate can relax tension when applied to affected areas. Used alongside mindful breathing and short walks, they can help mothers regain a sense of control.
Creating a supportive home environment
Family support is one of the strongest protectors against chronic pain and burnout. Shared chores, honest conversations, and setting limits on “mental load” tasks go a long way. Encouraging a mom to rest without guilt is not indulgent—it’s essential maintenance for the whole family.
Open discussions about mood changes or persistent pain can prevent misunderstandings and isolation. When symptoms interfere with daily life, pairing physical therapy with counseling or ADHD-focused coaching helps restore both balance and confidence.
FAQs
Q1: How can I tell if my pain is stress-related or something more?
Persistent pain lasting more than a few weeks, especially with fatigue, brain fog, or irritability, deserves a medical checkup. Pain linked to stress or ADHD often fluctuates with emotional load, but ruling out physical conditions is the first step.
Q2: Can hormonal changes really affect pain?
Yes. Estrogen influences how the body processes pain signals. When levels dip—during PMS, postpartum, or perimenopause—pain sensitivity often rises.
Q3: Is it safe to use topical pain relievers while breastfeeding?
Many topical products are considered safe when used correctly, but mothers should always confirm with a doctor. Some NSAIDs can be used cautiously under supervision, as noted by the NHS.
Q4: Do emotional support animals actually help with ADHD or pain?
Yes. Interaction with pets releases oxytocin, reduces anxiety, and offers emotional grounding. They’re not a cure but a valuable part of holistic stress management.
Q5: What’s the connection between ADHD and chronic pain?
People with ADHD are more prone to pain sensitivity due to how their nervous system processes stimuli. Managing ADHD symptoms often leads to better pain outcomes because it reduces overstimulation and tension.
Closing thoughts
Motherhood demands constant giving, but that doesn’t mean mothers must live in silent discomfort. Understanding how stress, hormones, and undiagnosed ADHD intertwine with chronic pain helps break the cycle of exhaustion. When families share the load, when mothers seek assessment and holistic care, and when small daily habits become moments of healing, the whole home benefits.